**
1. These amounts are before the deduction of Attorney fees and expenses.
2. This does not constitute a guarantee,warranty or prediction regarding the outcome of your case.
3. You may have to pay the opposing party's attorney fees and cost in the event of a loss.
FAILURE TO DIAGNOSE SEPSIS RESULTING IN DEATH: CONFIDENTIAL SETTLEMENT
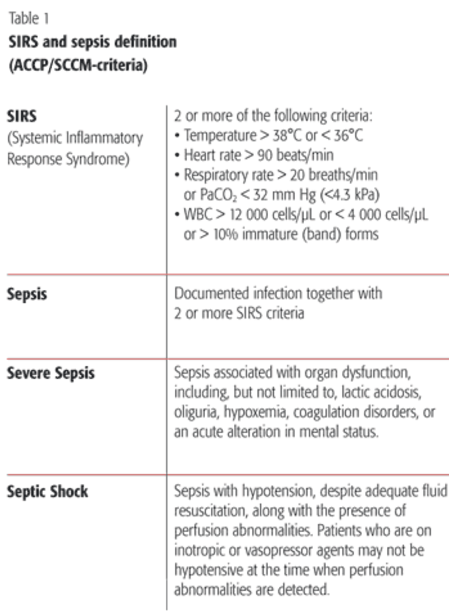
A 36 year old women flew to Las Vegas to visit a friend. While in Las Vegas, she began to feel ill. She went to the Hospital Emergency Room for treatment. In the Emergency Room, she was given fluids, diagnosed with the flu, and sent home. She was told to follow up with her own doctor in two days. In fact, she did not have the flu; she had Systemic Inflammatory Response Syndrome (SIRS). The emergency room doctor did not recognize the significance of the fact that she had two of the four signs for SIRS, (elevated pulse and temperature), coupled with her symptoms and complaints. Two signs for SIRS is the accepted criteria for presumed diagnosis, treatment, and hospital admission. The emergency room doctor let her leave the hospital with an elevated heart rate and temperature. He did not prescribe antibiotics, which would have saved her life. Two days later after being told she only had the flu, she decided to fly home to deal with her illness there. Her friend dropped her off at the airport. However, the airline would not let her board because she was too sick. Instead, they called an ambulance which transported her to the same Hospital Emergency Room. This time, she was seen by a different doctor. Now she had obvious signs of SIRS. All four clinical presentations for SIRS were present, including elevated temperature, heart rate, pulse, and respiratory rate. Still, the doctor was clueless that she had SIRS. To save her life, antibiotics and adequate intravenous fluids needed to be administered on an emergent bases upon presentation at the hospital. Unfortunately, appropriate life-saving interventions were not taken to treat the SIRS. Antibiotics were not administered until two hours after she arrived at the hospital. That was an unreasonable delay. Inadequate fluids were administered. They blew the chance to save her life. She died in the hospital. None of her doctors diagnosed her with SIRS until after she was dead. She died 10 hours after being admitted at the hospital in the intensive care unit.
I was able to successfully settle this case for a confidential amount.
UNNECESSARY SPINAL SURGERY ON A 26 YEAR OLD WOMAN WITH A NORMAL SPINE RESULTS IN PERMANENT PARALYSIS: CONFIDENTIAL SETTLEMENT
A 26 year old woman reported to her OB/GYN that she was experiencing back pain. She was referred to an orthopaedic surgeon. On her first visit with the surgeon the physical examination was essentially negative. He noted: “The patient walks with a normal gait. Heel walk is normal. Toe walk is normal. The patient walks without assistance. Regardless of these negative findings the surgeon told her on her very first visit that she needed extensive spinal surgery and hardware placements. In multiple medical reports the surgeon cited her recent MRI as the source of his diagnosis of severe stenosis, severe spondylolysis, herniated disc at L5-S1 and L5 fracture. He scheduled a follow up appointment in six weeks while he sought pre-authorization for surgery from her insurance company. The insurance company recommended her surgeon send her to pain management rather then surgery. The surgeon then concocted a scheme to bypass the insurance authorization process. He told the young lady to come to the emergency room the next day at the hospital while he was on duty and he would do the surgery on an emergency basis. She did as she was told. She was admitted on an emergency basis to the Hospital. The surgery was performed that day on an emergency basis without the need for insurance pre-authorization. The Surgical Request form states: “ PT admitted to the ER on an urgent basis. Surgeon was on call and did the above surgery. No Authorization needed when patient admitted to the Hospital through the Emergency Room.” The MRI was not available at the hospital for other doctors to confirm or refute the diagnosis made by the surgeon. The surgery was a disaster. The young lady woke up unable to move her legs and feet. Nurses notes state: “patient states she has no feeling from the waist down. Does not respond to painful stimuli of lower extremities.” A hospital discharge summary notes: “postoperatively the patient had no sensation or motor activity in the lower extremities. The patient was started on high dose steroid therapy. However, to date she still has not had any significant change.” The surgeon conceded: “I cannot explain why she has persistent pain.” She ended up to having to use a cane and wheelchair. She walks with an obvious limp and is in chronic pain. It turns out that the MRI taken before surgery showed no evidence of spondylolysis, no evidence of spinal stenosis, no evidence of disc protrusion or disc bulge and no fractures. The MRI demonstrates that she had a normal spine. She never needed spinal surgery and certainly not emergency spinal surgery with decompression and hardware. I was able to settle this case for a confidential amount.
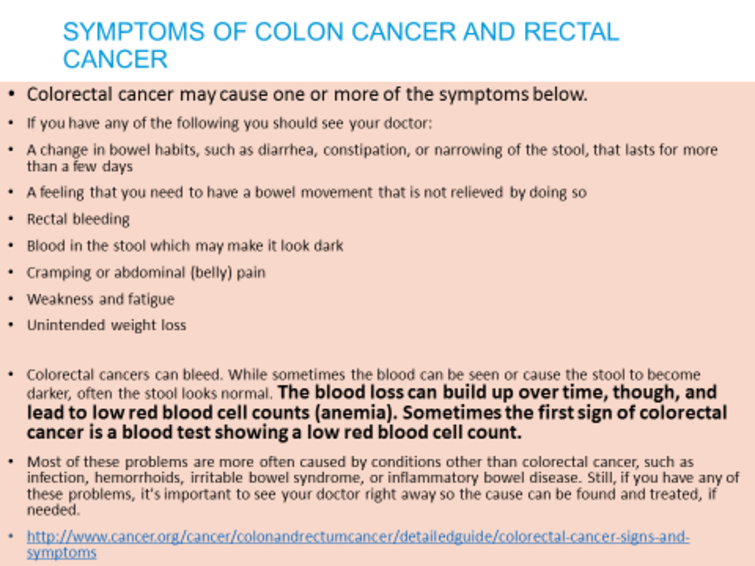
COLON RECTAL SPECIALIST IGNORES POSITIVE FINDINGS OF POLYPS ON BARIUM ENEMA REPORT AND BRIGHT RED RECTAL BLEEDING; FAILS TO PERFORM TESTING TO DIAGNOSE COLON CANCER RESULTING IN DEATH.
CONFIDENTIAL SETTLEMENT
A 72 year old man went to see a board certified colon rectal specialist because he was bleeding bright red blood from his rectum and having trouble going to the bathroom. He was sent for a barium enema test which showed 2 filling defects (polyps). The report recommended correlation with sigmoidoscopy. The barium enema findings were ignored by the specialist who never performed a sigmoidoscopy and did not send him for a colonoscopy. Instead the specialist treated him for hemorrhoids for six months. When the hemorrhoids stopped bothering him he stopped going for treatment. He was diagnosed with colon cancer 5 years later when he returned to the same doctor with more bleeding. He underwent resection surgery with complications and was forced to wear a colostomy bag for 2 years following surgery until the colon cancer finally killed him. The cancer could have been removed endoscopically without any surgery at all if the doctor had followed up with the re
DENTAL MALPRACTICE; DENTIST EXTRACTS TOOTH USING IMPROPER EQUIPMENT BLOWS UP PATIENTS FACE WITH AIR RESULTING IN PERMANENT NERVE DAMAGE AND DEEP JUGULAR VEIN THROMBOSIS: CONFIDENTIAL SETTLEMENT
A 27-year old woman presented to her dentist complaining of pain coming from two wisdom teeth, tooth #32 and tooth #1. The Dentist proceeded to extract both teeth. During the extraction a high speed air drill was used, forcing compressed air into the tissue at the extraction wound site. The compressed air caused her face to immediately swell. She heard an assistant ask the dentist: “Is it normal for her face to get that big? She was sent to the Hospital emergency room at hospital for evaluation after extractions.” The hospital noted: “The patient’s face is enormously swollen over the orbits and greater in the right face and neck.” A computerized tomography scan found extensive subcutaneous and soft tissue air is seen in the face bilaterally most marked in the cheek with air also seen in the right parapharygeal masticator spaces as well as air extending inferiorly along the facial planes between the neck musculature with air dissecting into the mediastinum . . . air is seen in two sockets of the right third upper lower molars. Impression was extensive soft tissue air as described with pneumomediastinum. The high-speed dental hand piece is operated by compressed air at high pressure. This drives a turbine in excess of 200,000 revolutions per minute. The tip of the burr, rotating at this speed generates frictional heat and requires cooling to avoid tissue burns. Cooling is commonly achieved using a separate jet of air and water directed onto the point of the burr. A number of modern high speed hand pieces have the ability to direct a mixture of air and water onto the burr with the driving gas to the turbine being directed away from the operative area. To avoid the possibility of introducing air into the tissues, oral and dental surgeons should use a low speed hand piece without the air/water spray and instead use a separate water or saline drip to cool the tissues and the burr tip and/or use a hand piece that exhaust air away from the surgical field. All of the medical literature makes this clear. The dentist office in this case did not have these types of drills. The inappropriate use of dental equipment caused the subcutaneous emphysema and the internal jugular vein thrombosis. During this emergency admission, a documented internal jugular vein thrombosis was discovered requiring 6 months of anticoagulant therapy. The internal jugular vein thrombosis was a direct result of the introduction of subcutaneous air into the right side of the neck. Deep jugular vein thrombosis (DVT) is a medical condition involving blood clotting. It is a disease process which forms thrombi that either partially or completely block circulation in a deep vein, generally in the lower extremities. Unlike the superficial veins just below the skin surface, the deep veins are surrounded by powerful muscles that contract to force blood back to the heart. One-way valves inside the veins prevent back flow of blood between muscle contractions. The quick and efficient return of blood to the heart using the power of the leg muscles is a crucial phase of the circulatory process. She was also diagnosed with right lingual nerve injury with paresthesia. “Cranial nerves show a 50% lingual nerve paresthesia. Neurosensory testing shows approximately a 50% paresthesia of the lingual nerve distribution.” This nerve damage is permanent. Her tongue feels constantly numb, she has no sense of taste, she drools frequently, has facial swelling, tooth aches and pain. In addition the lack of feeling causes her to accidentally bite her tongue. I was able to settle this case for a confidential amount.

SURGEON IMPROPERLY PLACES PEDICLE SCREW INTO THE NERVE OF 32 YEAR OLD WOMAN AND LEAVES IT THERE FOR 10 MONTHS CAUSING PERMANENT PARALYSIS IN BOTH LEGS: CONFIDENTIAL SETTLEMENT
A 32 year old woman presented to an orthopaedic surgeon who reported finding “a huge herniated fragment of L5-S1 and foraminal stenosis and lateral recess stenosis at L4-5.” His first operation was a failure During a second operation he placed pedicle screws and fusion cages into her back. However he failed to properly assess the correct placement of the pedicle screws. A third operation was performed with the pre-operative diagnosis of “pseudo-arthrosis of lumbar 4 through sacral 1. Loose internal fixation device lumbar 4 through sacral 1 with foraminal stenosis bilaterally lumbar 4 through sacral 1.” The third operation also failed to improve her condition. A CT scan showed incorrect placement of the pedicle screws at L4, with perforation of the medial pedicular wall on the left side resulting in invasion of the epidural space and impingement on the dural sac.” She had a fourth re-operation performed by a different surgeon. During that operation “stenosis was noted at L4-5 and in the L5 foramen” and that a pseudomeningocele was found “over the left L4 root.” Pseudomeningoceles are collections of spinal fluid that communicate with the CSF space that surrounds the spinal cord. The CSF of the pseudomeningocele is surrounded by paraspinous soft tissues. Because they have no confining membrane pseudomeningoceles tend to enlarge as more and more fluid escapes from the subarachnoid space into the soft tissue pseudomeningocele. The doctor also discovered considerable scar tissue. The fourth operation was also unsuccessful and the doctor had a great deal of difficulty attempting to repair the pseudomeningocele at L4. The Surgeon failed to properly assess her deteriorating condition He allowed the improperly placed pedicle screw at L4 that was pushing on her nerves to remain for a period of approximately 10 months. The impinging screw at L4 caused nerve damage and tearing of the dura which led to the development of a pseudomeningocele at L4. Her condition was made worse following four surgeries. She is now totally disabled and suffers from permanent nerve root damage resulting in pain, weakness, and sensory impairment in both lower extremities.
I was able to settle this case for a confidential amount.

DOCTOR PERFORMS SPINAL SURGERY IN A RUSH THEN ABANDONS HIS PATIENT WITHOUT CHECKING ON HER. HE FAILED TO ANSWER HIS PAGES FROM THE HOSPITAL FOR TWO HOURS. MEANWHILE HE ALLOWED HER TO BLEED INTERNALLY IN THE RECOVERY ROOM. THIS RESULTED IN HER PERMANENT PARALYSIS AND LOSS OF BLADDER AND BOWEL FUNCTION. CONFIDENTIAL SETTLEMENT
A 71 year old semi-retired woman went to her doctor with a diagnosis of spinal stenosis (Stenosis is typically caused by the aging process of the spine). The doctor noted that “The patient walks with a normal gait. Heel walk is normal. Toe walk is normal. The patient walks without assistance.” The doctor recommended that she undergo a laminectomy (spinal surgery) to relieve her spinal stenosis. He performed a laminectomy from L2-S1 under general anesthesia completing this extensive operation in only 46 minutes. He did not have another doctor assist with the surgery but only a physicians assistant. Immediately following the surgery she was unable to move her legs at all. She also reported loss of bladder control. She has never recovered from this condition. The surgeon did not verify that she could not move her legs in the Recovery Room. The nurses noted severe pain and discomfort and they tried to contact surgeon. They placed pages at 12:30, 12:45, 13:15 and 13:45. His office was called directly. Finally at 14:00 the doctor called back. He took no measures, and did not return to see the patient that day. She was given repeated doses of 2mg of morphine IV every 10 minutes for a total of 16 mg plus 1 mg of Versed IV at 12:30, 12:45 and 13:28. The anesthesiologist wrote: right leg weak, numb with 3 strength at arrival to post anesthesia care unit, surgeon had left operating room already. Did not answer page, ordered number to page every 10 minutes. Patient was discharged to ward with this serious neurological deficit.
The doctor did not examine his patient, in the recovery room, he failed to answer his pages for almost 2 hours and when he was finally notified he failed to conduct an examination to find out the cause of the problem. On a later visit he wrote: “I know during the surgical procedure there were no problems. I cannot explain her current symptoms.” He then wrote in the discharge summary that the patient had an uneventful hospital course. Nerve conduction studies were performed by a different doctor. His report stated: “There is nerve injury inside the spinal canal where the nerve comes off the spinal cord. Circulation of the spinal cord or traction pressure on cord could produce this problem . . .” Another report notes: “Her nerve conduction studies showed a pattern of radicular changes in the distribution of right L5-S1 and left L5 radiculopathy. Features may well be vascular or traction response to the [spinal] cord.” An MRI report found clumping of the nerve roots. A neurologist then diagnosed her with Arachnoiditis, (inflamation of the membrane surrounding the nerve roots) status post spine surgery and peroneal palsy. The report states “MRI done in May showed clumping of the nerve roots at L3-L5, with some sort of spinal cord displacement.” Significantly, physical examination noted that: “Motor nerve conduction studies show no response in the lower extremities and the absence of an H-reflex.” The clumping of the nerve roots and the nerve injury were not present on the MRI taken before surgery. The spinal damage was caused by damaging the spine and nerve roots during surgery. The surgeon fell below the standard of care of a competent surgeon both during and following surgery. He failed to take proper steps to care for his patient following surgery. He allowed her to bleed internally in the recovery room. This has resulted in her permanent paralysis and loss of bladder and bowel function. Because of her medical condition she rarely ventures into public. On the rare occasions when she does leave her home she is required to wear diapers because she cannot control her bladder or bowel functions. She spends her days confined to a small room inside of her home. I was able to settle this case for a confidential amount.

57 YEAR OLD WOMAN WITH SEVERE SLEEP APNEA IS GIVEN AN IMPROPER PRESCRIPTION FOR PROMETHAZINE WITH CODEINE; KILLING HER IN HER SLEEP
CONFIDENTIAL SETTLEMENT
A 57 year old woman who suffered from severe sleep apnea died in her sleep. Her immediate cause of death was listed as “acute combined multiple drug intoxication”. All of her prescriptions were prescribed by the same doctor. She had a sleep study done at a clinic two years before her death. Following the study, it was recommended that she should not be given any sedatives and a list of other dangerous medications, because of her sleep apnea. Her doctor ignored these recommendations and prescribed these drugs anyway. He never warned her they could kill her. The Coroner’s Toxicology Report showed Codeine, Hydrocodone, Alprazolam, and Gabapentin in her bloodstream, all of which are sedating medications proscribed by her doctor. Of all of his improper prescriptions, the worst was Promethazine with Codeine. Promethazine with Codeine is a syrup used as a cough suppressant. Promethazine is also very sedating. Because of potential respiratory depression, it carries specific warnings not to use in persons with sleep apnea. The doctor knew she had severe sleep apnea. This drug is only supposed to be given temporarily (a few days). The doctor gave her this drug in massive dosages for four months, far in excess of the recommended dosage, until if finally killed her. On every exam in the month prior to her death the doctor found that her lungs were clear. There was no complaint of a cough or finding of a cough recorded in the records. The office notes did not even show a Promethazine with Codeine prescription. However, a verbal prescription was uncovered (from the pharmacy) from the doctors office, for Promethazine with Codeine, called to the Pharmacy for “cough”. It was refilled a month later despite a lack of any complaints of cough being noted in the medical records. The doctor admitted in his deposition that the woman was not a drug addict, not clinically depressed and that she was not suicidal. She was married with 4 adult children when she died.
The case was settled for a confidential amount

Specialist repeatedly fails to investigate the cause of 41 year old womans low iron anemia. The doctor never did a sigmoidoscopy or a colonoscopy. That was medical malpractice and the cause of her untimely death.
CONFIDENTIAL SETTLEMENT
1,2,3
A 41 year old woman died from metastatic colon cancer. She sought medical attention from a gastroenterolgist, where she received numerous abnormal lab results indicating she had anemia and low iron anemia.
Low iron anemia is a red flag warning sign for colon cancer. Iron is needed to make hemoglobin, the protein that delivers oxygen to tissues throughout the body. A deficiency can be caused by all sorts of conditions that are not cancer, including heavy menstrual periods, ulcers, and a diet that is too low in iron. Because since iron-deficiency anemia can also be evidence of colon cancer, it is essential that doctors take steps to find out the specific cause.
As a specialist, the gastroenterologist and his medical staff should have picked up on the significance of her symptoms, particularly her low-iron anemia. He should have done a proper investigation and examination. A specialist acting within his or her specialty is held to a higher standard. Specialists are "expected to exercise that degree of skill, learning and care normally possessed and exercised by the average physician who devotes special study and attention to the diagnosis and treatment" of diseases within that specialty.
PATIENT FALLS OUT OF BED WHILE TRYING TO GO TO THE BATHROOM RESULTING IN ABOVE THE KNEE AMPUTATION. FALL RISK PROTOCOLS WERE VIOLATED BY HOSPITAL AND NURSING STAFF. GUARD RAILS WERE NOT RAISED AND THE NURSING STAFF IGNORED CALL LIGHT.
CONFIDENTIAL SETTLEMENT
Patient was admitted to a Rehabilitation Hospital Corporation for 6 weeks of antibiotic therapy. He was classified upon admission as a high risk for falls because of his amputee status. ).
He was assigned as a patient to Nurse P. Nurse P administered 15 milligrams of Lortab to Patient. The nurse testified at her deposition as follows:
Q. What was his condition when you left?
A. He was fine, he was resting and he was all right.
Q. Was the patient, restrained in any manner?
A. No.
Q. Were guardrails up on the bed?
A. Not in the daytime.
Q. Were the bed wheels locked down?
A. I do not remember that. (Nurse P).
Q. Do you know whether or not the guardrails were raised on his bed ever?
. . ..THE WITNESS: Yes
Q. When were they raised on his bed?
A. Well, that morning I did not see the guardrails raised on his bed. I do not exactly remember.
Q. How about when you left his room and when you administered drugs at 1300, 1;00, were the guardrails raised then?
A. I believe one side was up and the other side he has a table in front of him.
According to the director of nursing the Hospital terminated Nurse P for poor performance. "I swear to God that I terminated this young lady . . ." (
At approximately 3:00 p.m. Patient was discovered lying on the floor next to his bed by the nursing supervisor, nurse S. . . . I was doing my round when I went by and saw that he was on the floor.@ (Nurse S. A
". . . I went down with all my strength and my stub just splattered it was like somebody dropped a watermelon, blood went all over the walls and stuff. And I started screaming for help." Patient
Nurse S discovered that the bed had rolled away while Patient was attempting to transfer himself from his wheelchair to his bed. . . . He told me that he went to go to bed and the bed rolled away from him. That=s why he fell.@ (Nurse S).
Q. Had the bed rolled like he said it did?
A. Yes, because I did check the bed. Yeah the bed rolled
Q. . . . And was the bed in a position that was consistent with what he told you?
A. Yeah, the bed rolled.
Q. It does roll?
A. Yes.
Q. And did you see that it had rolled away from where his chair was?
A. Yeah. (Nurse S).
Patients wife arrived at the Hospital and discovered him still on the floor. ". . .I went directly to his room and he was on the floor. There was blood smear on the floor. There was two or three nurses in the room standing around. He was in terrible pain." "His bed was pushed to the . . . other side of the room."
Nurse S did not inspect the wheels on the bed to see if they were locked. However, she did push the bed and the bed rolled). Patient fell during a change in the nursing shift. (Nurse S) ". . . he was bleeding through his stump." (Nurse S).
If the person is in bed and they're high risk for falls both side rails are supposed to be up. (Nurse S). Nurse S testified that if she would have seen that one of the side rails on the bed was not raised while he was in bed she would have told nurse P to raise the siderail. ". . . if I see that it's down, I would." (Nurse S).
According to the nursing Director, Patient was allowed to transfer himself as desired before his fall at the Hospital.
A. Well, here it says that he was alert and oriented, up in wheelchair to bathroom as desired.
Q. Okay. Does that mean he's allowed to get up out of his bed and go to the bathroom anytime he wants to?
A. It would appear that way.
Q. It does. So, he would not be noncompliant for getting up out of the bed himself.
A. It does not look this way.
You said a moment earlier he was allowed to get up and go to the bathroom as desired so wouldn't you agree that would lead him to believe that he was able to get up and out of bed as desired as well to go to the snack bar or get up and out of bed as desired?
A. I would assume that, yeah.
The Nursing Director agreed the, bed wheels should have been locked at all times. "That is standard protocol in any facility you work on so the beds don't move. The beds are on wheels. You want to make sure they're secure."
Q. Would you expect a bed to roll away if the bed wheels were locked and somebody pushed on the bed?
A You would expect that it would not . .
The care plan was changed after his fall.
Q. . . . What changes were made, what modifications were made?
A. In addition to the initial one which stated elevated rails especially at night, all light within reach, and position of bed at normal level, they added keep wheels locked at all times and encourage patient to cal for assistance to transfers.
Following the fall Patient was transported by ambulance to a full service Hospital. Patient described his pain as "terribly painful". Surgery was then performed. According to the operative report "The patient's left leg was prepped and draped in the usual manner. The 15 cm defect which the traumatic wound dehiscence had caused was carefully scrubbed out and old hematoma was removed. There was no evidence of infection. Cultures were taken. The flaps were then slightly debrided and then reclosed with 32 monofilament nylon sutures. Dr. S characterized the fall as major trauma to the stump.
Patient was unable to sleep for weeks following surgery due to the pain. He was basically confined to his bed during this period. According to Dr. S everything was done to try to save his knee and nothing worked.
A knee disarticulation was performed by Dr. S. According to Dr. S the loss of the knee resulted in a loss of mobility . ". . . One thing he has lost is his ability to control that knee. So if it involves, for instance bending or crouching down, he may have more difficulty with those types of lifting maneuvers."
Expert witness Dr. H explained why Patent lost his knee as follows:
He had his revision by Dr. S. He had an uneventful recovery and one week later was discharged . There is no evidence that he was having anything more than the usual and customary postoperative pain in the stump at that time.
He sustained the fall, three days later, ten days after the original surgery. At that time, he broke the wound open, contused the end of his stump, and he had quite severe pain from what I understand from the records, had to have it irrigated and closed again. .
So for, a period of five months, he has had three operations on his stump and an operation on his hip. That's an awful lot of trauma to an area. So it doesn't surprise me at all that he was having the degree of pain he had.
It's also my opinion that there was a degree of reflex sympathetic imbalance in this extremity, and that was due to the trauma he had sustained in that leg from hip to knee, so that doesn't surprise me too much= especially the fact that there was a crushing injury to the stump, because crushing injuries or explosion-type injuries tend to have a higher incidence of reflex sympathetic dystrophy. So that's my opinion on why he had the pain and why he had the knee disarticulation.
After the fall at he could not stand up more than one hour at a time. He fell down four times in front of people at work. He could no longer functions at work. He had several falls on the job. He was told no other positions were available for him. He decided to resign.
After he lost his knee and his job he became very depressed.
After reviewing the entire chart, the director of nursing, testified in her deposition on this particular instance in this particular chart there was not adequate charting done..
Q. So, it's below the hospital protocol for charting?
A. In this particular instance it doesn't meet the standard, you're correct.
Throughout the chart there were numerous places where the nurses were supposed to document that the side rails in the bed were placed up. Yet these portions of the chart were left completely blank.
Q. And those were all supposed to be filled out, right?
A. Yes.
"A form is supposed to be filled out and by not filling it out it means it wasn=t done . . .
The patients care plan for was not checked off by the assigned nurse as having been reviewed.
Q. The fact that this is blank, not signed, initialed, or anything else, that=s not standard operating procedure?
A. I would have to say yes, she should have reviewed that section. Is that your question?
Q. Yes. That=s my question. Not to do is not the standard operating procedure of the hospital, right?
A. No. She should have reviewed her care plan. .
According to the Director, ". . . we had not had a good fall policy." " . . . I couldn=t find anything in writing about a fall policy".
A . . .I thought we needed to have a good fall restraint policy because I didn't find anything like that when I first got there.
Q. So you decided to implement new fall prevention protocol policies and did that after {this} fall, right?
a. It just happened because I was reviewing all the policies and procedures many of which were not what I thought were not what I thought were acute enough that we needed to look at because of my background and so I went through the quality manager and our committee to say we need to improve on this process and have a policy.
Q. Right. And you also had somebody fall in the hospital and get hurt?
a. Yeah.
Q. Shortly after the hospital opened up?
a. I also had just taken over that job as well and as part of my duty to preview policies and procedures and start to begin to implement because this facility was not being run as an acute care facility. It should have been. There was a lot of nursing home type mentality there. We were getting sicker and sicker patients there and we needed to have policies and procedures.
Q. What do you mean it should have been as an acute type facility to paraphrase your words as best as you can?
a. Of the philosophy of admission to this facility it=s a different licensure. It=s called a long-term acute facility. When you use the term long-term care, many people assumed that long-term care meant like a nursing home would be and it was not.
We were taking acutely ill people out of intensive care and so a lot of policies and procedures needed to be looked at and that=s why I was hired because my predecessor was not looking at those particular areas when she first came she was only there one month and then I took the position.
They had many forms just protocols that were meant like real nursing home type stuff and rehab stuff and that=s not what we were and I needed to get back to that acute care 24-hour nursing care so I was in the beginning process of starting to change those things not just because he fell and I was getting - -
Q. Well, you say not just because.
a. That's the indication I got from you.
Q. You already said you believed the prevention policies were not adequate and you had a fall in the hospital so certainly that was an additional cause or reason for revamping the policies.
a. I would agree with that, yes.
Nurse P the assigned nurse on did not review the patients care plan on that day. Patient was allowed to transfer himself as desired even though he was high risk for falls because of his amputee status and the fact he was taking narcotics. This was a violation of their own policy. The bed wheels were not locked down on the bed. The bed wheels were supposed to be locked at all times. Both the side rails on were not raised to prevent him from self transferring. This was another violation of the Hospitals own policy.
Q. Well, if the guard rails are both up, that discourages the patient obviously from getting in and out of bed on their own.
a. Absolutely.
Q. So, obviously that could have prevented him from self-transfer?
a. It would, yeah. He couldn't get out of bed if the side rails - - I wouldn't think he could being an amputee.
The Hospital allowed an amputee under the influence of a large dosage of narcotics to self transfer at will. They did not lock the wheels down on his bed. This caused the bed to roll away and Patient to fall on his stump. They did not keep the side rails on the bed raised up. This would have prevented self transferring and would have prevented this tragic fall.
Ex Felon in Possession of a Firearm
Client was charged with ex felon in possession of a firearm. He was facing 10 years in prison. He had a wife and family and did not want to go to prison. He carried a gun for self defense as he has to live and travel thru some bad neighborhoods. I fought the case based on an invalid police search involving an inventory search of his car. The police claimed they did an inventory search prior to impounding the vehicle; but they did not fill out an inventory form of the vehicles contents. (the only item they mentioned in reports was the gun they found). Police also claimed there was a loose cushion in the back seat, however they used a crow bar to get the back seat up. All charges were eventually dropped. Case dismissed. Client happy.